RBS: Harnessing the Power of Lean Six Sigma to Reduce Costs and Complications of Chest Tube Clogging
All stakeholders in healthcare want to see improved outcome and reduced costs to maximize patient value. The question is how to get there? As promising new technologies and protocols are innovated and become known, the questions are always the same:
- “How do we know this works?”
- “Is it worth it to make the changes in protocols needed to figure this out?”
- “Is there return on investment given the costs and time to implement it?”
Thousands of companies, and now hospitals, have turned to Lean Six Sigma to improve quality and reduce costs through a specified process to answer these questions. In particular, the Lean process is designed to eliminate non-value add activities and reduce waste while maximizing customer value. The Six Sigma process can facilitate this through quantitative problem solving.
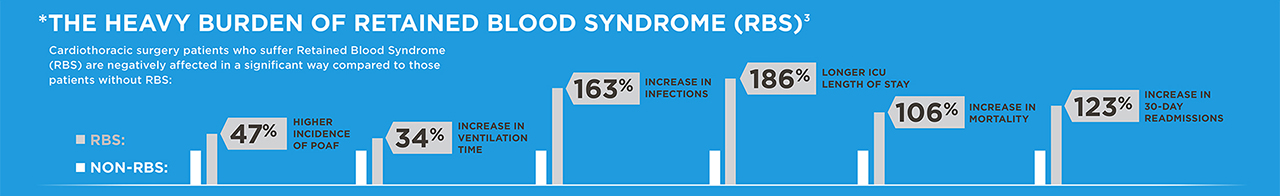
Some of the best targets are common processes with considerable variability. Once such process, common to all heart and lung surgery patients, is the ICU management of chest tubes. Chest tubes are used on every case, nearly without exception. The purpose of a chest tube is to remain patent while in use. Chest tubes, however, can clog in as much as 36% of patients. When chest tubes clog, it can result in Retained Blood Syndrome (RBS), which leads to complications and increased costs.
There exists considerable variability in how chest tubes are currently managed to prevent chest tube clogging and thus no standard approach to reduce RBS. Nearly every hospital, every shift and sometimes every nurse has a different approach. Current methods to maintain patency includes stripping and milking, which is not shown to work and may be harmful, as well as breaking the sterile seal and suctioning the chest tubes in the non-sterile ICU environment. Thus, this is ripe for Lean Six Sigma approaches to improve process. Innovations to improve chest tube patency, such as Active Clearance Technology, now exist with promising published results. But where do you start to make sure the value is realized for implementing this technology?
Using Six Sigma in a formal continuous quality improvement setting, first define and measure the problem (RBS). This can easily be done with existing administrative data using ICD-9 and ICD-10 codes. Second, develop and implement a formal chest tube patency standard for the ICU. Standardization allows for better workflow, more efficient resource utilization, and more reliable and measurable outcomes. Next, analyze the results, and adjust if needed. 
A step-by-step program that combines Lean Thinking with the concepts of Six Sigma in a clinical protocol process improvement methodology for chest tube management can measure the improvements both clinically and economically. Such a program is available that pools the power of the waste reduction focus of Lean Enterprise and the variation reduction techniques of Six Sigma.
As a case study was published in the Journal of Thoracic and Cardiovascular Surgery (link to Sirch Article), where such a program reduced RBS by 43%, as well as a Postoperative Atrial Fibrillation (POAF), a problem triggered in part by RBS, by 33% by using this methodology to implement an active chest tube patency maintenance program. Isn’t it time your program consider harvesting the power of six sigma for your ICU management of chest tubes?